Not affiliated with The United States Office of Personnel Management or any government agency
Federal Employee Retirement and Benefits News
MENUMENU
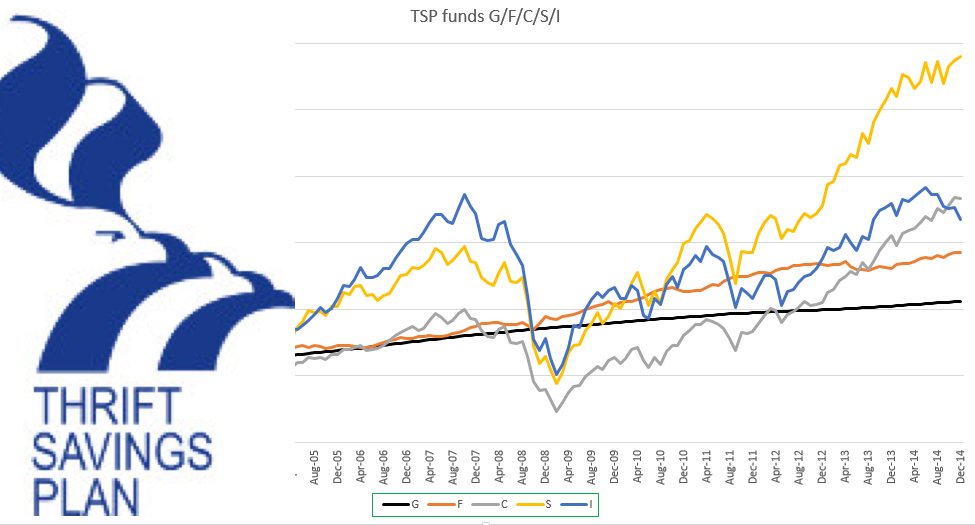
- Thrift Savings Plan
-

Advertisement
-
- FERS
-
- Latest News
- Retirement for Postal Workers: Everything you need to know | Michael Wood
- Defense Department Reports On Take-Rates Projections For BRS
- TSP and Divorce: How The Court Will Handle Your TSP and Other Federal Benefits | Linda Jensen
- Battle Regarding Official Time and TSP Takes Place On Capitol Hill
- Linda Jensen | How You Can Successfully Fund Your Retirement Years
- Latest News

Advertisement
-
- CSRS
- Federal Employee Annuities
- Financial Planning
- Newsletter